The Disease
The incubation time (the time from exposure to first symptoms)
usually ranges from 1-6 days, although cutaneous cases have
been reported as long as 60 days after exposure.
There are three major anthrax syndromes in humans
- Cutaneous anthrax
- Inhalational anthrax
- Gastrointestinal anthrax
Cutaneous anthrax
When anthrax spores are introduced into the body through a
break in the skin, they multiply and spread locally. The release
of three toxins - edema factor, lethal factor and protective
antigen - leads to tissue swelling and necrosis (cell and
tissue death).
Three to five days after exposure, a small, painless, itchy
bump develops in the exposed area (usually face, neck, arms,
hands). The lesion then develops into a vesicle and finally
an ulcer with a characteristic black centre. There is often
significant swelling associated with the skin lesion. Left
untreated, and small but significant proportion of cases may
progress to systemic infection and even death. Treatment with
antibiotics, however, is very effective in preventing systemic
illness.
 |
Cutaneous Anthrax Infection of the Hand
and Cheek
Photos taken from the New England Journal of Medicine.
Panel A shows the characteristic blackened eschar
surrounded by eroded areas and massive edema. These
lesions are painless. The areas of "dried skin" represent
resolving edema. Lesions continue to progress despite
rigorous antibiotic treatment. Cutaneous anthrax
can be self-limiting, and the lesions resolve without
scarring. About 10 percent of untreated cutaneous
anthrax infections progress to systemic
anthrax. Panels B, C, and D show
changes in the lesion on the cheek over a seven-day
period. The characteristic blackened eschar is present
on day 0 (Panel B). Facial edema and ulceration occur
by the second day (Panel C). On day 7, the lesion
is beginning to heal, and the facial edema is resolving
(Panel D). |
Inhalational anthrax
Anthrax spores inhaled into the lungs are taken to regional
lymph nodes in the chest. Multiplication of the organism leads
to inflammation and destruction of these lymph nodes and spread
into the bloodstream.
Early diagnosis of inhalation anthrax is difficult, as the
initial symptoms are non-specific and flu-like (fever, muscle
ache). However, these symptoms rapidly progress two to three
days later, with the development of low blood pressure (shock)
and respiratory problems such as shortness of breath. At this
point, the disease is usually fatal even if antibiotic therapy
is started.
Gastrointestinal anthrax
Gastointestinal anthrax is extremely rare. It most often occurs
as multiple cases in households following the consumption
of contaminated meat. Microscopic examination of intestinal
tissue reveals inflammatory infiltrates, ulceration and swelling
similar to that of cutaneous anthrax. Symptoms are variable
and include fever, vomiting, abdominal pain, bloody diarrhea
and the accumulation of fluid in the abdominal cavity. Death
occurs from intestinal perforation or shock from fluid imbalances.
Reported mortality rates range from 25% to 75%.
 |
 |
B. anthracis is a large, nonmotile, gram-positive
aerobic rod capable of forming spores. It is a member of a
group of bacilli that are encountered in the laboratory as
a normal skin contaminant. B. anthracis can be differentiated
from the other bacilli in this group morphologically and through
biochemical testing.
Anthrax is diagnosed by isolating B. anthracis from
skin lesions, sputum, abdominal fluid or feces depending on
the suspected anthrax syndrome. The organism is almost always
found in the blood. Detection of anthrax antibodies in the
blood is also possible.
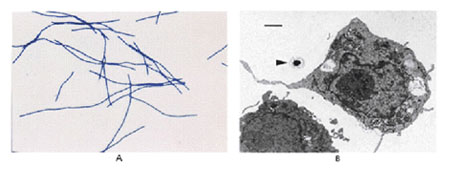 |
Photomicrographs of Bacillus
anthracis Vegetative Cells and Spores
Photos taken from the New England Journal of Medicine
Panel A shows a Gram's stain of B. anthracis
vegetative bacteria. The bacterial cells exhibit gram-positive
staining (purple filaments) (x600). Panel B shows an
electron photomicrograph of a B. anthracis
spore (arrowhead) partially surrounded by the pseudopod
of a cultured macrophage (x137,000). The bar represents
1 µm. |
B. anthracis can be treated by a variety of antibiotics.
Penicillin, chloramphenicol, tetracycline, erythromycin, streptomycin
or ciprofloxacin can be used. As many of the symptoms of anthrax
are mediated by toxin release, the role of antitoxins in the
management of inhalational anthrax infection is under investigation.
However, there are no preparations currently available. Antibiotic
administration to asymptomatic patients after an exposure
to anthrax is also recommended.
|